In the new 2018 Quality Payment Program (QPP) Final Rule, the Centers for Medicare and Medicaid Services (CMS) has outlined a wide range of changes to its value-based care programs. Are you and your EHR vendor prepared?
2018 marks the second year of the Merit-Based Incentive Payment System (MIPS), and the requirements are definitely ramping up and posing more of a challenge. However, CMS' MIPS is nothing to be too scared of--as long as your practice has the right technology to streamline your MIPS data collection and submission.
So what's specifically changing? In case you don't have time to read all 1,653 pages of the 2018 Quality Payment Program Final Rule yourself, here's an overview:
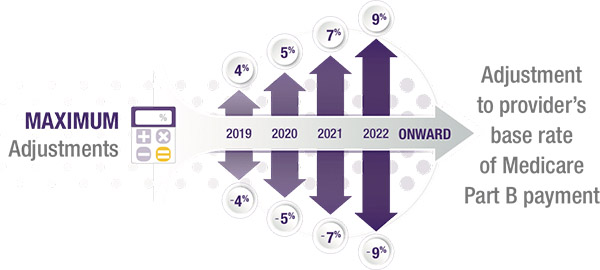
Payment adjustment increases to +/-5 percent.
CMS is raising the stakes for 2018--if only by 1 percent. This past year, providers could earn up to a 4 percent positive or negative adjustment on their Medicare reimbursements (applied in 2019) depending on their MIPS performance, but that percentage increases to +/-5 percent for 2018 (applied in 2020).
This means that if your practice bills $1,000,000 in Medicare per year, then your MIPS performance could earn you a $50,000 bonus or penalty in 2020. And since the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) requires CMS' MIPS program to be budget-neutral, that bonus could increase by an additional adjustment factor if more providers earn a negative adjustment than anticipated.
Low-volume threshold goes up
In 2018, providers with ≤$90,000 in Part B allowed charges or ≤200 Part B beneficiaries will not be subject to MIPS. Compared to the 2017 MIPS threshold of ≤$30,000 in charges or ≤100 beneficiaries, this is a significant increase. The 2017 threshold already exempted a large proportion of Medicare Part B providers, and this 2018 change will exempt even more.
 Performance threshold increases to 15
Performance threshold increases to 15
For the 2017 performance period, providers could avoid the negative Medicare payment adjustment in 2019 with a MIPS Composite Performance Score (CPS) of just three points. This could be easily achieved by submitting either one Quality measure, one Improvement Activity (IA) or all Promoting Interoperability (PI; formerly Advancing Care Information) base measures.
For the 2018 performance period, you'll need 15 points or more to avoid the negative adjustment in 2020. While this is a 400% increase, it could still be as simple as completing 2-3 Quality measures, four IAs or all PI base measures. For practices that are already strong MIPS performers, this minimum threshold change will have little impact. The exceptional performance threshold required for positive adjustments will remain at 70 points.
Cost category takes effect
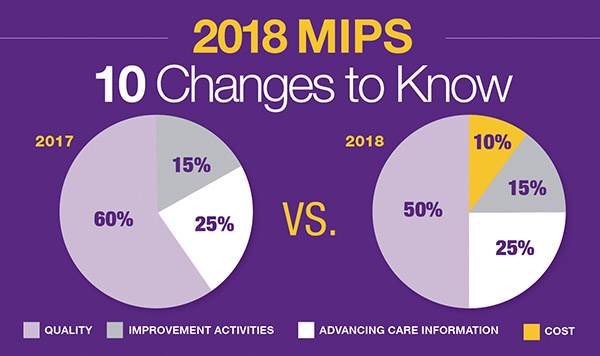
In its first year, MIPS scored providers on three categories: Quality, PI and IA, with the Cost category weighted at 0%. Starting in 2018, MIPS adds a 10 percent weight for the Cost category, which is based on Medicare Part B claim submissions. Because eligible clinicians (ECs) already submit this claims data to CMS, they will not need to send any additional data to report the Cost category.
More specifically, Cost scoring is based on the Medicare spending per beneficiary (MSPB) and the total per capita costs for all attributed beneficiaries measure. This could have an enormous impact on the scores of clinicians who frequently prescribe expensive Part B drugs, such as ophthalmologists, rheumatologists and oncologists. We'll take a closer look at the Cost category in an upcoming blog post, so stay tuned!
Category weights change
The Quality category was originally proposed to remain at 60 percent of the MIPS CPS in 2018, with Cost not factoring in until 2019. However, the 2018 QPP Final Rule introduced Cost this year at 10 percent, so CMS is decreasing Quality's weight to 50% to compensate. The PI and IA categories will remain at 25 and 15 percent, respectively.
Virtual group participation option introduced
With many small practices concerned about their ability to succeed independently under MACRA and MIPS, CMS has introduced a virtual groups option that can allow ECs to benefit from group reporting without actually joining a group or selling their practice.
To form a MIPS virtual group in the Quality Payment Program, a solo practitioner or group of 10 or fewer ECs must come together virtually with at least one other solo practitioner or group to participate in MIPS for a year. Group members do not need to be in the same specialty or location. CMS simply requires that they report as a group across all performance categories and meet the same MIPS requirements as non-virtual groups.
Once MIPS reporting is complete, all group members will receive the same score and Medicare payment adjustment percentage. The idea is that by sharing the reporting burden and combining their strengths, providers may be able to earn higher MIPS scores together than individually.
To learn more, download CMS' MIPS Virtual Groups Toolkit.
Extreme and uncontrollable circumstances exemption added
In the wake of Hurricanes Harvey, Irma and Maria, CMS has added new hardship exemptions for physicians who cannot meet MIPS reporting requirements due to hurricanes, natural disasters or public health emergencies. These will apply to the 2017 Quality Payment Program performance year as well as 2018, and the application deadline for hardship exceptions will be December 31 each year.
How does it work? If affected clinicians don't submit any data, they will be exempt from penalties. Meanwhile, those who do submit data will be scored on the data they submit, but the categories will be reweighted. If you were impacted in 2017, you may submit an application for reweighting of the PI category. Even if you don't submit a PI application, CMS will automatically exempt you from Quality, Cost and IA for 2017.
Small practice bonus instituted
In an effort to further reduce the MIPS reporting burden for small practices, CMS will automatically award qualifying practices a bonus of up to 5 points. Practices must have 15 or fewer ECs and submit data on at least one performance category to be eligible.
2014 CEHRT permitted and 2015 CEHRT bonus created
Originally, CMS planned to allow 2018 MIPS data submission only from 2015 Certified Electronic Health Record Technology (CEHRT). Instead, it has now decided to continue allowing ECs to use 2014 CEHRT--a relief for both vendors and providers. However, CMS is offering a 10 percent bonus in the PI category to providers who report with 2015 CEHRT.
 New ePrescribing and HIE exclusions established starting 2017
New ePrescribing and HIE exclusions established starting 2017
To allay concerns about the difficulty of meeting certain measures involving ePrescribing and health information exchange (HIE), CMS has introduced new exclusions that would allow ECs to claim the exclusion from one or both of those measures and still earn a base score. It's important to note that these exclusions are being applied to the 2017 performance year as well as 2018.
Who's eligible? To claim the eRx exclusion, a provider or group must write fewer than 100 permissible prescriptions during the reporting period. For the HIE exclusion, they must refer or transition fewer than 100 times during the reporting period.
Analysis
With these new rules, CMS is continuing to ramp up the reporting requirements as planned, building up to full MIPS implementation in 2019. In response to concerns from the healthcare community about the burden of Quality Payment Program reporting, CMS is also focusing heavily on easing the transition and accommodating real clinical workflows.
Especially for small practices, the new Quality Payment Program rules provide additional flexibility and incentives in a wide variety of areas. As a result, some organizations have actually criticized CMS for not challenging providers enough to substantially improve health outcomes or reduce costs. However, for many physicians and industry associations, this relative leniency comes as a major relief.
To learn more and view the full list of calendar year (CY) 2018 MIPS changes, check out CMS' 2018 Quality Payment Program Final Rule fact sheet.
The Bottom Line
Value-based care is here to stay, but it's reassuring to see that CMS continues to listen to feedback from the healthcare community. And ultimately, meeting these new MIPS requirements doesn't require an enormous amount of time and resources - it just comes down to whether you have the right tools.
With the performance periods for Quality and Cost beginning on January 1 for all MIPS-eligible clinicians, now is a good time to evaluate whether your current EHR system will be able to support your MIPS success in 2018. A robust MIPS solution should be able to collect reportable MIPS data during the exam, track and benchmark your CPS in real time and submit your data directly to CMS. Plus, consider augmenting your technology with personal guidance from certified MIPS coaches who are also experts in your EHR system. When you're equipped with comprehensive MIPS support tools from a proven MIPS performer, you can gain peace of mind while helping increase your Medicare income.
 Jayne Collard is the Manager of Advisory Services at Modernizing Medicine and is a Certified MIPS Health Professional (CMHP). She leads an EMAzing team of MIPS Advisors for both EMA and gMed while living and working out of Colorado.
Jayne Collard is the Manager of Advisory Services at Modernizing Medicine and is a Certified MIPS Health Professional (CMHP). She leads an EMAzing team of MIPS Advisors for both EMA and gMed while living and working out of Colorado.
Reprinted with permission from Modernizing Medicine.
Modernizing Medicine and its affiliated companies empower physicians with suites of mobile, specialty-specific solutions that transform how healthcare information is created, consumed and utilized to increase practice efficiency and improve patient outcomes. Built for value-based healthcare, Modernizing Medicine's data-driven, touch- and cloud-based products and services are programmed by a team that includes practicing physicians to meet the unique needs of dermatology, gastroenterology, ophthalmology, orthopedics, otolaryngology, pain management, plastic surgery and urology practices, as well as ambulatory surgery centers. For more information, please visit www.modmed.com.